A tiny chip implanted into the eyes of people suffering vision loss from irreversible age-related macular degeneration has restored central sight in a dazzling first.
It's called the PRIMA system, tested across 17 European hospitals, and it restored central vision in 26 of 32 patients who used it for 12 months – many of whom could even read again. The result, developed by a large international team of doctors and scientists over many years, represents a massive breakthrough in treatments for vision loss.
"It's the first time that any attempt at vision restoration has achieved such results in a large number of patients," says ophthamologist José-Alain Sahel of the University of Pittsburgh School of Medicine, co-senior author on a paper describing the results.
"More than 80 percent of the patients were able to read letters and words, and some of them are reading pages in a book. This is really something we couldn't have dreamt of when we started on this journey, together with Daniel Palanker, 15 years ago."
Related: Gold Injections in The Eye May Be The Future of Vision Preservation

Geographic vision loss from age-related macular degeneration is a progressive and irreversible condition that affects millions of people around the world. The macula, which is responsible for high-resolution central vision, resides within the retina at the back of the eye. As this part of the retina trophies, patches of blindness develop in a person's central vision.
In a healthy retina, photoreceptor cells convert light into electrical signals that are processed in the inner retina and sent to the brain. For people with geographic atrophy, these photoreceptor cells die off, which means that part of the eye is not receiving light signals, creating a blind spot in the center of their vision, while peripheral vision is less affected.
While not everyone with age-related macular degeneration will experience geographic atrophy, for the millions that do, it can be devastating.
PRIMA, the brainchild of ophthalmologist Daniel Palanker of Stanford University, co-senior author of the research paper led by ophthalmologist Frank Holz of the University of Bonn in Germany, could be poised to change that.
The system consists of two parts. The implant is a tiny wireless silicon sensor, just two by two millimeters in area and less than the width of a hair in thickness, and containing 378 photovoltaic pixels. It's slipped in behind the retina where the cellular atrophy is greatest.
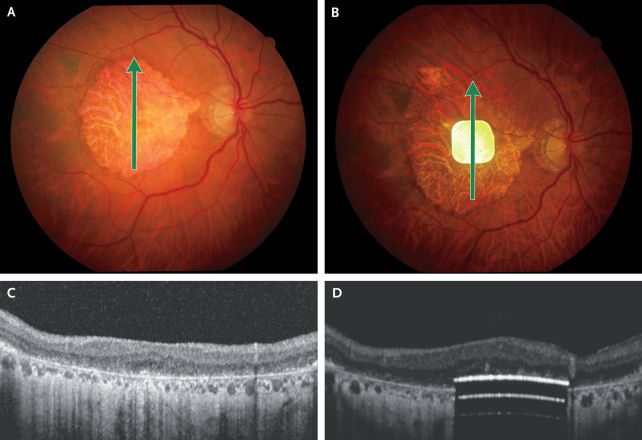 The eye of a patient before and after implantation of the photovoltaic array. (Holz et al, NEJM, 2025)
The eye of a patient before and after implantation of the photovoltaic array. (Holz et al, NEJM, 2025)The other part of PRIMA is a pair of glasses connected to a pocket processor. The glasses capture images and convert them into near-infrared light near the 880-nanometer wavelength before sending them to the implant. The wavelength is important: near-infrared light is invisible to the human eye, so it will not be perceived by the healthy retinal photoreceptors or interfere with the patient's remaining peripheral vision.
The implant, in turn, converts the infrared signals into electrical signals and sends them to the brain to be perceived, similar to how the natural eye converts and transmits data. And because the implant is powered by light, it doesn't need an external power source.
After extensive clinical testing and a small, five-participant clinical trial, the researchers were ready for the next step. They recruited 38 patients in 17 hospitals across five European countries to test the system for 12 months; six of those patients were unavailable for follow-up at the end of the trial period, so the results are based on the remaining 32 patients.
The mean age of the patients was 79, and all were experiencing vision loss from geographic atrophy. Their vision was tested before undergoing the trial, and again at several points during the trial. Initially, the patients had to spend several months learning how to use PRIMA, including the functions of the system, such as zooming in on text, and interpreting the electrical patterns as visual shapes.
Most of the patients – 26, or 81 percent – experienced a clinically meaningful improvement in their vision, with some patients even reaching vision close to 20/420, the resolution limit of the PRIMA system.
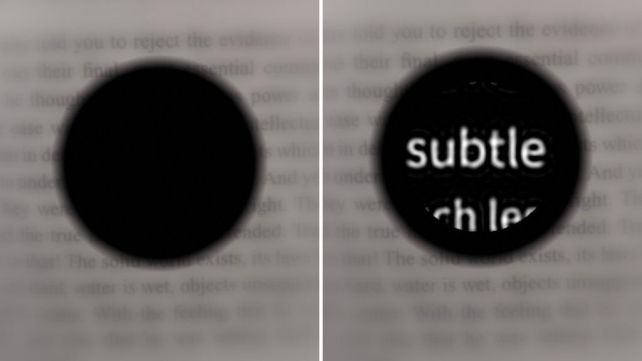 Simulations of a macular degeneration patient's vision before (left) and after (right) implantation of the PRIMA system. (Palanker Lab)
Simulations of a macular degeneration patient's vision before (left) and after (right) implantation of the PRIMA system. (Palanker Lab)"Before receiving the implant, it was like having two black discs in my eyes, with the outside distorted," says patient Sheila Irvine, who was recruited to the trial at Moorfields Eye Hospital in the UK.
"I was an avid bookworm, and I wanted that back. I was nervous, excited, all those things. There was no pain during the operation, but you're still aware of what's happening. It's a new way of looking through your eyes, and it was dead exciting when I began seeing a letter. It's not simple, learning to read again, but the more hours I put in, the more I pick up."
It's important to note that 19 of the participants experienced adverse effects, all of which are known complications of eye surgery, and most of which were resolved quickly. Crucially, peripheral vision remained unaffected in all patients.
Currently, PRIMA only works in black-and-white. The researchers are working to develop a grayscale version and to increase the resolution of the system.
"Number one on the patients' wish list is reading, but number two, very close behind, is face recognition. And face recognition requires grayscale," Palanker says.
"This is the first version of the chip, and resolution is relatively low. The next generation of the chip, with smaller pixels, will have better resolution and be paired with sleeker-looking glasses."
The research has been published in the New England Journal of Medicine.

.jpg) 10 hours ago
3
10 hours ago
3

 English (US)
English (US)