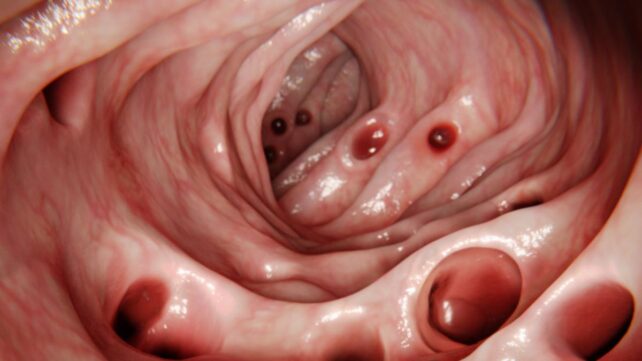
 Small pouches in the gut wall can become inflamed. (selvanegra/Getty Images)
Small pouches in the gut wall can become inflamed. (selvanegra/Getty Images)
It's easy to see your body aging on the outside – wrinkles, dark spots, gray hair, the whole shebang – but as we grow older, our insides also inevitably change.
By the time most people reach the ripe age of 80, the smooth lining of their digestive tract is scattered with small, bulging pouches of tissue.
These sac-like protrusions along the digestive tract, called diverticula, are 'weak spots' in the gut's muscular wall. They are typically harmless, and most people never even know they are there.
Related: A Single Data Point at Age 7 Could Predict How Long You'll Live
Sometimes, after a colonoscopy, patients are alarmed to find they have developed diverticulosis, but most of the time, this condition is nothing to worry about.
Watch the video below for a summary on this condition;

Only if the pouches become inflamed or infected is it considered diverticular disease, or diverticulitis. Symptoms, which generally come and go, often include constipation, diarrhea, abdominal pain, bloating, or fever.
"It certainly doesn't help that the names are similar, so it can be confusing," gastroenterologist Janyll Castineira from the University of Miami explained in July this year.
"I try to help my patients remember that diverticul'O'sis are p'O'ckets and diverticul'I'tis is 'I'nflammation."
 Some people with diverticular disease will experience uncomfortable symptoms. (Sora Shimazaki from Pexels/Canva)
Some people with diverticular disease will experience uncomfortable symptoms. (Sora Shimazaki from Pexels/Canva)The good news is that even if a person does develop diverticulitis, their symptoms usually improve with just a few days of bed rest and a liquid diet. Over 85 percent of patients find this sufficient.
No one knows exactly what causes diverticula to form in the first place, but current treatments generally focus on helping the digestive tract move smoothly, without blockages.
That's why a high-fiber diet, including between 25 and 30 grams of fiber a day, is often recommended to recovering patients. This won't heal existing diverticula, but may prevent more from forming.
How long poop stays in your body could have more profound implications for your overall health than a first glance would suggest.
According to a 2023 review that brought together data from dozens of studies, distinct differences can be seen between the gut microbiomes of 'speeders' and 'slowpokes'.
Since the human gut microbiome is intrinsically linked to health, this could have implications that have gone unnoticed before now.
Related: Your Gut's Methane-Making Microbes Could Secretly Turn Fiber Into Extra Calories
 Mild diverticulosis is common and can often go undetected. (Wan & Kristo, Clin. Geriatr. Med., 2021)
Mild diverticulosis is common and can often go undetected. (Wan & Kristo, Clin. Geriatr. Med., 2021)According to the United Kingdom's National Health Service (NHS), people aged 50 to 70 who eat a diet high in fiber have a 40 percent lower risk of hospitalization from diverticular disease compared to people with the lowest fiber intake.
Today, it is still unknown how fiber and other gut influencers, such as antibiotics or probiotics, may impact how the pouches initially form. According to a 2024 review, these factors remain controversial and warrant further investigation.
Diverticulosis, however, is very common in Western countries such as the US, Australia, and the UK, where diets are low in fiber, and relatively rare in Africa and Asia, where diets are higher in fiber.
Other potential risk factors include obesity, lack of exercise, and smoking. There's likely a complicated mix of contributing factors.
 Examples of diverticula in the gut. (Harvard University)
Examples of diverticula in the gut. (Harvard University)While diverticula can develop in the large and small intestine, around 95 percent of patients in the Western world have diverticula in their sigmoid colon.
This part of the digestive tract works under great pressure to push feces into the rectum.
Once diverticula form, possibly from excessive pressure, they are prone to bleeding when aggravated, in a similar way to hemorrhoids, which form inside and outside the rectum and around the anus.
Diverticular bleeding is estimated to cause between 30 and 65 percent of all cases of lower gastrointestinal bleeding. It's usually painless and self-limiting, but seeing blood in the stool is a serious matter, as it may indicate other severe conditions.
Related: A Type of Fiber May Have Weight Loss Benefits Similar to Ozempic
Experts advise that those who notice blood in the stool seek immediate medical guidance, even if they suspect it is related to diverticula.
Diverticulosis can typically be diagnosed with a CT scan or colonoscopy.
Surgery is only needed in severe cases – for instance, those in which an abscess forms or ruptures.
Yet even then, the outcomes after surgery are excellent. Roughly 90 percent of patients do not show symptoms again after the most troublesome part of their intestine is removed.
Related: A Rare Cancer Is Surging in Young People, And Experts Are Puzzled
"Treatment depends on the severity of the episode," says gastroenterologist Francesca Raffa from the University of Miami.
"Most cases are mild and can be treated in an outpatient setting. Your provider will likely recommend a liquid diet at first, over-the-counter pain medications, and will determine if an antibiotic course is appropriate."
If only all the signs of aging were as easy to manage.

.jpg) 1 hour ago
2
1 hour ago
2

 English (US)
English (US)