 A CPAP mask system is the current first-line treatment for sleep apnea. (Grandriver/E+/Getty Images)
A CPAP mask system is the current first-line treatment for sleep apnea. (Grandriver/E+/Getty Images)
Obstructive sleep apnea, a breathing disorder where the airway becomes blocked during sleep, comes with numerous health risks and dangers – but a potential new treatment could make a real difference to the millions of people affected worldwide.
The new approach, described in a study by researchers at Flinders University in Australia, builds on an existing treatment called hypoglossal nerve stimulation (HNS). The hypoglossal nerve controls the tongue, and HNS uses electrical pulses to prevent the tongue from blocking the throat.
However, as it stands today, HNS requires surgery and a relatively bulky implant – it's invasive and time-consuming. It also doesn't work for everyone. Here, researchers wanted to test a smaller electrode that's easier to insert and manage.
Bottom line: it worked. In brief stimulation trials lasting several breaths, the new HNS electrode effectively opened the airway on 13 out of the 14 participants tested – a 93 percent success rate. In some cases, it was even successful when breathing had stopped completely. The early signs are that this is a substantial upgrade for HNS.
"It's a 90-minute procedure performed under ultrasound guidance with minimal discomfort," says otolaryngologist Simon Carney, from Flinders University.
"Importantly, we were able to open airways in patients previously considered unsuitable for HNS."
While the approach will need further development and testing before it can be used more widely, ultimately it promises an HNS treatment option that could be implanted through a short procedure in a clinic, rather than via more invasive surgery (with its associated risks) at a hospital.
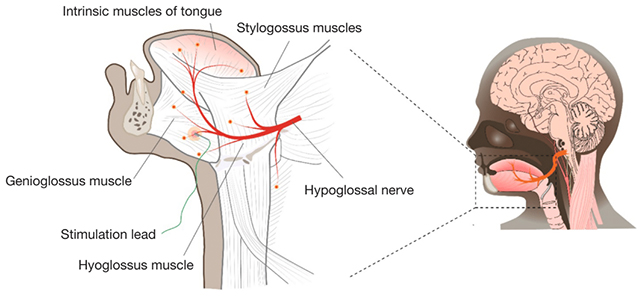 The treatment focuses on the hypoglossal nerve, pictured here in red. (Osman et al., Chest, 2026)
The treatment focuses on the hypoglossal nerve, pictured here in red. (Osman et al., Chest, 2026)That means it would be an option for more people with obstructive sleep apnea (OSA). Eligible patients could be seen more quickly and would have less recovery time than with surgery.
Currently, HNS is largely effective, but not always, and the researchers say their new version could be tailored more precisely for individuals. Being a less invasive procedure, it should be easier to tweak.
HNS isn't actually the first line of treatment against OSA though: that's something called Continuous Positive Airway Pressure or CPAP. This beats HNS in its results overall, but it involves wearing a mask over the mouth during sleep to keep the airway open.
It's a rather awkward setup, despite its effectiveness, and about half of patients find they're able to tolerate CPAP and stick with it. That's where HNS comes in, and the new and improved version that the researchers have tested here.
"This approach may reduce recovery time and costs, while improving success rates for people who cannot tolerate conventional treatments," says physiologist and lead author Amal Osman, from Flinders University.
The team says their next steps are to develop this approach so it can be used safely and practically in the long term and integrate it with wearable technologies. Other nerves and muscles could potentially be targeted to improve airflow as well.
It's worth noting that this was a study carried out in a sleep lab, with a relatively small group of people with OSA. The initial findings are very encouraging, but the technique needs to be tested with more people and in more natural settings.
There's clearly plenty of need for more treatments for OSA. The condition can seriously disrupt sleep – so crucial for maintaining physical and mental health – and has been associated with raised risk for cardiovascular disease and dementia.
Whether it's reducing the risk of cognitive decline in people with OSA or simply helping them to feel less tired throughout the day, improved treatments could make a major difference – and this new take on HNS is off to an encouraging start.
Related: The FDA Just Approved The First US Drug Treatment For Sleep Apnea
"Our goal is to give patients more choices and better outcomes," says Danny Eckert, from Flinders University.
"This study shows that with innovation and the right tools, sleep apnea treatment can become more accessible, comfortable, personalized, and effective."
The research has been published in Chest.

.jpg) 2 hours ago
2
2 hours ago
2

 English (US)
English (US)